Thoracic Aortic Aneurysm Imaging: Overview, Radiography, Computed Tomography
Overview
Thoracic aortic aneurysm represents aneurysmal dilatation of the ascending thoracic aorta, the aortic arch, or the descending thoracic aorta. Aortic aneurysm is defined as a localized or diffuse dilatation of more than 50% normal diameter of the aorta. It occurs with the highest frequency of all of the diseases of the thoracic aorta that require surgical treatment. Better imaging technology has led to the earlier recognition of acute aortic dissection, permitting the identification of more patients with complex conditions who are candidates for surgery.
Below are 2 images depicting thoracic aortic aneurysm.
 Chest radiograph showing widening of the superior mediastinum.
Chest radiograph showing widening of the superior mediastinum.  Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium.
Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium. Anatomy
Thoracic aneurysms are classified in accordance with the portion of aorta involved: the ascending thoracic aorta, the arch, or the descending thoracic aorta. This anatomic distinction is important because the etiology, natural history, and treatment of thoracic aneurysms vary for each of these segments.
The DeBakey and Stanford classifications are the 2 most widely used methods of describing the types of aortic dissection. In the DeBakey classification, there are 3 types of dissection: types I, II, and III; dissections are classified on the basis of the origin and extent of the dissecting process. In the Stanford system, type A signifies involvement of the ascending aorta, with or without involvement of the arch or the descending aorta (regardless of the site of the primary intimal tear). Type B represents all others, or dissections that do not involve the ascending aorta.
The aortic layers, beginning at the innermost wall, are the intima, the media, and the adventitia. In aortic dissection, a tear in the intima allows blood to escape from the true lumen of the aorta. The inner later of the media is rapidly dissected from the outer layer, and blood causes the aorta to rapidly expand above normal size. A false channel forms in the outer half of the aortic media, whose walls are exceedingly thin and are highly susceptible to rupture. Size is an important predictor of the risk of aneurysm rupture.Chronic dissections are generally diagnosed 2 weeks after the initial tear and may expand in the weakened aortic wall to develop an aneurysm.
Aneurysms of the descending aorta are most common, followed by aneurysms of the ascending aorta; aneurysms of the arch occur less often. In addition, descending aortic thoracic aneurysms may extend distally to involve the abdominal aorta and create a thoracoabdominal aortic aneurysm. Sometimes, the entire aorta may be ectatic, with localized aneurysms seen at sites in both the thoracic and abdominal aorta. Interestingly, thoracic aortic aneurysms are less common than aneurysms of the abdominal aorta.
Preferred examination
Although aortic dissection may be suspected on the basis of history and physical findings, diagnostic imaging is necessary to establish the diagnosis. A clear and efficient imaging strategy is required. The clinical team involved in the diagnosis and treatment of patients with aortic dissection should prospectively agree on a strategy. In developing an approach, consideration should be given to the technology available at the institution and the ease of performing each test, especially after hours.
The preferred examinations for diagnosis are aortic angiography, magnetic resonance imaging (MRI), magnetic resonance angiography (MRA), and echocardiography.
Aortography was the criterion standard against which other modalities were measured, but with the advent of transesophageal echocardiography (TEE) and computed tomography scanning (CT), this modality is now rarely used; however, aortography is still the preferred modality for the preoperative evaluation of thoracic aortic aneurysms and for precise definition of the anatomy of the aneurysm and great vessels.
CT scanning is a reliable modality for diagnosing aortic dissection; this modality is the diagnostic method of choice in most institutions. CT scans usually show dilation of the aorta, an intimal flap, and both the false and true lumina. Rapid scanning after an intravenous bolus injection of contrast material allows the detection of differential filling rates in the true and false lumina.
TEE is helpful, owing to the proximity of the esophagus to the aorta; with this modality, higher transducer frequencies may be used to better delineate the aorta. TEE is highly sensitive but less specific, and it is excellent at detecting pericardial effusion and aortic regurgitation. TEE may be quickly performed at the patient's bedside with the patient under sedation; it does not expose the patient to radiation, nor is the injection of contrast material necessary. However, it may be difficult to evaluate the ascending aorta and the proximal arch with TEE.
MRI is useful in defining thoracic aortic anatomy and detecting aneurysms; this modality is particularly useful for patients with preexisting aortic disease. MRI is an appealing option in the detection of aortic dissection. Sensitivity and specificity are excellent, but it is time consuming and cumbersome to perform.
MRA may prove especially useful in defining the anatomy of aortic branch vessels.
Limitation of techniques
TTE is not accurate for diagnosing thoracic aneurysms, and it is particularly limited in its ability to examine the descending thoracic aorta. TEE is a far more accurate method for assessing the thoracic aorta and has become widely used for detection of aortic dissection. There has been less experience with TEE, however, in the evaluation of nondissecting thoracic aneurysms.
TEE, CT scanning , and MRI have been reported to be highly sensitive for the diagnosis of aortic dissection. However, the specificity of CT scanning and MRI is significantly better than that of TEE.
Differential diagnosis and other problems to be considered
Acute myocardial infarction and pneumothorax are included in the differential diagnosis. Other conditions to be considered are acute coronary syndrome, pulmonary embolism, acute pericarditis, pericardial effusion or tamponade, new aortic regurgitation, penetrating aortic ulcer, aortic intramural hemorrhage, esophageal rupture, and musculoskeletal and/or spinal conditions.
Special concerns
In patients with aortic aneurysm, aortic dissection is the most feared catastrophic event. Rupture of a thoracic aortic aneurysm is more frequent than abdominal aortic rupture. Thus, high clinical suspicion is required, and time is of the essence. Imaging techniques, including MRI, TEE, or CT scanning, should be quickly utilized.
Radiography
Many thoracic aneurysms are readily visible on chest radiographs. Characteristic findings are (1) widening of the mediastinal silhouette, (2) enlargement of the aortic knob, or (3) displacement of the trachea from the midline (see the first image below).
 Chest radiograph showing widening of the superior mediastinum.
Chest radiograph showing widening of the superior mediastinum.  Chest radiograph in a patient with a thoracic aortic aneurysm following aneurysm surgery.
Chest radiograph in a patient with a thoracic aortic aneurysm following aneurysm surgery. Chest radiographs display abnormalities in 80-90% of patients, but the abnormalities are nonspecific. For example, mediastinal widening occurs in more than 75% of cases and may occur in the ascending aorta, the aortic arch, or the descending portion of the thoracic aorta. This finding may be difficult to differentiate from the aortic tortuosity that is associated with long-standing hypertension. Up to 12% of patients with aortic dissection have a normal chest image.
The calcium sign is a rare radiographic finding in aortic dissection. Generally, intimal calcification is seen along the outer border of the aorta. With dissection of the aortic media, the calcium deposit becomes separated from the outermost portion of the aorta by more than 0.5 cm.
Other radiographic signs include a double-opacity appearance of the aorta, with the suggestion of true and false channels; a localized bulge along a normally smooth aortic contour; a disparity in the caliber between the descending and ascending aorta; obliteration of the aortic knob; and displacement of the trachea to the right by the dissection.
Degree of confidence
The degree of confidence is moderate.
False positives/negatives
Unfortunately, smaller aneurysms, especially saccular ones, may not be evident on the chest radiograph. Therefore, this technique cannot exclude the diagnosis of aortic aneurysm.
Computed Tomography
On CT scans, thoracic aortic aneurysms are characterized by an increase in aortic diameter and outward displacement of calcium of the aortic wall (see the images below). CT scanning is an effective method for defining the maximum diameter of the aneurysm and monitoring the diameter over time. A diameter exceeding 4 cm is considered aneurysmal. A diameter exceeding 6 cm is usually an indication for surgery of thoracic aortic aneurysm.
 Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium.
Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium. 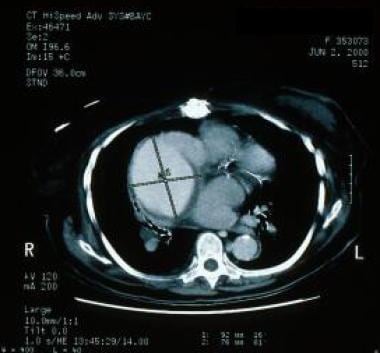 Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm.
Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm. Established linear methods for measuring aortic size include reviewing cross-sectional dimensions in the axial plane and double oblique plane. A small study comparing the 2 methods found that at all locations the double oblique plane yielded smaller differences with planimetry than the axial plane and differed with the axial plane in proportion to aortic geometric obliquity.
Degree of confidence
The degree of confidence is high.
False positives/negatives
The rates of false-positive and false-negative findings are low.
Magnetic Resonance Imaging
MRI and CT scanning are now the modalities most frequently used for diagnosing and monitoring thoracic aortic diseases.
A number of reports attest to the effectiveness of MRI for the evaluation of both true and false aortic aneurysms. Velocity-encoded cine MRI provides a measurement of the differential flow velocity in the true and false channels. By using multiple images per cardiac cycle, a velocity-time curve may be generated to display the disparate flow pattern in the 2 channels.
MRI and MRA are used to monitor the maximum diameter and extent of the thoracic aortic aneurysm. A maximum diameter exceeding 6 cm indicates the need for surgical repair. Regular monitoring is important for patients with Marfan syndrome and other conditions associated with progressive aortic dilatation.
Velocity-encoded cine MRI may be used to quantify the volume of concomitant aortic regurgitation in patients with aortoannular abnormalities.
Gadolinium warning
Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Systemic Fibrosis. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans.
NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public Health Advisory or Medscape.
Degree of confidence
The degree of confidence is high. Because MRI and MRA are noninvasive and provide images along both the short and long axes of the thoracic aorta, these modalities are now the preferred method for the follow-up of patients with thoracic aortic diseases. MRA in the sagittal plane is effective for depicting the origins of the arch branches and visceral arteries of the abdominal aorta and their relationship to the aneurysm.
False positives/negatives
The rates of false-positive and false-negative findings are low.
Ultrasonography
Transesophageal echocardiography (TEE) provides an assessment of cardiac structure and function and is highly sensitive in the diagnosis of aortic pathologies.This modality is reliable for surveys of the following:
- Aortic valve disease
- Aortic dilatation
- Ascending aortic aneurysm
- Aortic dissection
- Thrombi
- Atherosclerotic disease
- Mitral valve disease
Intraoperatively, TEE may be used to monitor cardiac function; detect atherosclerosis in the thoracic aorta; establish the competency of the aortic valve before surgery; and lower the incidence of stroke, by enabling surgeons to better navigate the placement of clamps and to avoid loosening any atherosclerotic plaques, which could otherwise cause brain embolism.
Degree of confidence
The degree of confidence is high. The accuracy of TEE in imaging intimal membranes for signs of aortic dissection has been reported to be 90%.
False positives/negatives
TEE poorly depicts aneurysms below the diaphragm and in the transverse aortic arch. In addition, this modality requires a skilled cardiologist to interpret the study data, because a high rate of false-positive results has been observed with those who are unfamiliar with the diagnostic limitations of TEE.
Angiography
The findings of aortic dissection seen at angiography include the following: (1) filling of a false channel with or without an intervening intimal flap, (2) distortion of the true lumen by either a patent or a thrombosed false lumen, (3) thickening of the aortic wall by more than 0.5 cm from a thrombosed false lumen, and (4) displaced intimal calcification.
Aortography is accurate for determining the site of the intimal tear and the extent of the dissection (see the first image below). Aortic regurgitation is also easily demonstrated with aortography; this modality demonstrates the extent and location of dissection into aortic side branches.
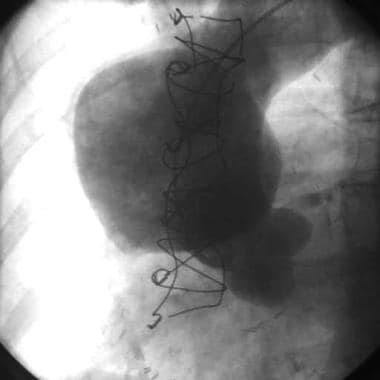 Ascending aortogram showing ascending aortic aneurysm. The patient also underwent computed tomography scanning.
Ascending aortogram showing ascending aortic aneurysm. The patient also underwent computed tomography scanning. 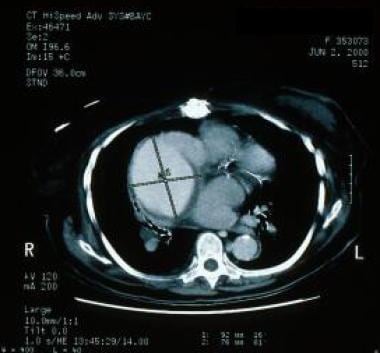 Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm.
Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm. Generally, all patients electively undergo aortography. It is used in the assessment of operative risks and in deciding on possible modifications of operative technique. The aortogram depicts aortic root dilatation and clearly defines the geography of the aorta and the condition of the smaller vessels. Absolute indications for aortography include renovascular hypertension, intermittent claudication, atherosclerotic occlusive abdominal aorta, and symptoms of carotid stenosis.
Cardiac catheterization may be required to evaluate any concomitant atherosclerotic occlusive disease of the coronary arteries, which may be corrected before or at the same time as the aortic aneurysm.
Degree of confidence
Aortography is highly specific. However, it is an invasive procedure, and it increases the risk of renal failure, owing to the use of radiopaque dyes.
False positives/negatives
False-positive and false-negative findings are rare.
Vibhuti N Singh, MD, MPH, FACC, FSCAI Clinical Assistant Professor, Division of Cardiology, University of South Florida College of Medicine; Director, Cardiology Division and Cardiac Catheterization Lab, Chair, Department of Medicine, Bayfront Medical Center, Bayfront Cardiovascular Associates; President, Suncoast Cardiovascular Research
Vibhuti N Singh, MD, MPH, FACC, FSCAI is a member of the following medical societies: American College of Cardiology, American College of Physicians, American Heart Association, American Medical Association, Florida Medical Association
Coauthor(s)
Paula M Novelli, MD Assistant Professor, Department of Radiology, Division of Vascular and Interventional Radiology, University of Michigan Health System
Paula M Novelli, MD is a member of the following medical societies: American College of Radiology, American Roentgen Ray Society, Society of Interventional Radiology
Specialty Editor Board
Bernard D Coombs, MB, ChB, PhD Consulting Staff, Department of Specialist Rehabilitation Services, Hutt Valley District Health Board, New Zealand
David S Levey, MD Orthopedic and Neurospinal MRI, Forensic Diagnostic Radiologist; President, David S Levey, MD, PA, San Antonio, Texas
David S Levey, MD is a member of the following medical societies: International Society of Forensic Radiology and Imaging, Forensic Expert Witness Association, Technical Advisory Service for Attorneys, Bexar County Medical Society, Texas Medical Association
Chief Editor
Eugene C Lin, MD Attending Radiologist, Teaching Coordinator for Cardiac Imaging, Radiology Residency Program, Virginia Mason Medical Center; Clinical Assistant Professor of Radiology, University of Washington School of Medicine
Eugene C Lin, MD is a member of the following medical societies: American College of Nuclear Medicine, American College of Radiology, Radiological Society of North America, Society of Nuclear Medicine amd Molecular Imaging
Anthony Watkinson, MD Professor of Interventional Radiology, The Peninsula Medical School; Consultant and Senior Lecturer, Department of Radiology, The Royal Devon and Exeter Hospital, UK
Anthony Watkinson, MD is a member of the following medical societies: Radiological Society of North America, Royal College of Radiologists, Royal College of Surgeons of England
References
- Coselli JS, Conklin LD, LeMaire SA. Thoracoabdominal aortic aneurysm repair: review and update of current strategies. Ann Thorac Surg. 2002 Nov. 74(5):S1881-4; discussion S1892-8. [Medline].
- Gott VL, Cameron DE, Alejo DE, et al. Aortic root replacement in 271 Marfan patients: a 24-year experience. Ann Thorac Surg. 2002 Feb. 73(2):438-43. [Medline].
- Mitchell RS. Stent grafts for the thoracic aorta: a new paradigm?. Ann Thorac Surg. 2002 Nov. 74(5):S1818-20; discussion S1825-32. [Medline].
- Rachel ES, Bergamini TM, Kinney EV, et al. Endovascular repair of thoracic aortic aneurysms: a paradigm shift in standard of care. Vasc Endovascular Surg. 2002 Mar-Apr. 36(2):105-13. [Medline].
- Saccani S, Nicolini F, Beghi C, et al. Thoracic aortic stents: a combined solution for complex cases. Eur J Vasc Endovasc Surg. 2002 Nov. 24(5):423-7. [Medline].
- Cheng SW, Lam ES, Fung GS, Ho P, Ting AC, Chow KW. A computational fluid dynamic study of stent graft remodeling after endovascular repair of thoracic aortic dissections. J Vasc Surg. 2008 Aug. 48(2):303-9; discusion 309-10. [Medline].
- Crimi E, Lee JT, Dake MD, van der Starre PJ. Transesophageal echocardiography guidance for stent-graft repair of a thoracic aneurysm is facilitated by the ability of partial stent deployment. Ann Vasc Surg. 2012 Aug. 26(6):861.e7-9. [Medline].
- Davies RR, Goldstein LJ, Coady MA, et al. Yearly rupture or dissection rates for thoracic aortic aneurysms: simple prediction based on size. Ann Thorac Surg. 2002 Jan. 73(1):17-27; discussion 27-8. [Medline].
- Lin MP, Chang SC, Wu RH, Chou CK, Tzeng WS. A comparison of computed tomography, magnetic resonance imaging, and digital subtraction angiography findings in the diagnosis of infected aortic aneurysm. J Comput Assist Tomogr. 2008 Jul-Aug. 32(4):616-20. [Medline].
- Miller WT. Thoracic aortic aneurysms: plain film findings. Semin Roentgenol. 2001 Oct. 36(4):288-94.
- Chryssidis S, Davies RP, Tie ML. Gadolinium-enhanced computed tomographic aortography. Australas Radiol. 2002 Mar. 46(1):97-100. [Medline].
- Nguyen BT. Computed tomography diagnosis of thoracic aortic aneurysms. Semin Roentgenol. 2001 Oct. 36(4):309-24. [Medline].
- Methodius-Ngwodo WC, Burkett AB, Kochupura PV, Wellons ED, Fuhrman G, Rosenthal D. The role of CT angiography in the diagnosis of blunt traumatic thoracic aortic disruption and unsuspected carotid artery injury. Am Surg. 2008 Jul. 74(7):580-5; discussion 585-6. [Medline].
- Mendoza DD, Kochar M, Devereux RB, Basson CT, Min JK, Holmes K, et al. Impact of image analysis methodology on diagnostic and surgical classification of patients with thoracic aortic aneurysms. Ann Thorac Surg. 2011 Sep. 92(3):904-12. [Medline].
- Lankipalli RS, Pellecchia M, Burke JF. Magnetic resonance angiography in the evaluation of aortic pseudoaneurysm. Heart. 2002 Feb. 87(2):157. [Medline].
- Pereles FS, McCarthy RM, Baskaran V, et al. Thoracic aortic dissection and aneurysm: evaluation with nonenhanced trueFISP MR angiography in less than 4 minutes. Radiology. 2002 Apr. 223(1):270-4. [Medline].
- Roberts DA. Magnetic resonance imaging of thoracic aortic aneurysm and dissection. Semin Roentgenol. 2001 Oct. 36(4):295-308. [Medline].
- Backes WH, Nijenhuis RJ, Mess WH, Wilmink FA, Schurink GW, Jacobs MJ. Magnetic resonance angiography of collateral blood supply to spinal cord in thoracic and thoracoabdominal aortic aneurysm patients. J Vasc Surg. 2008 Aug. 48(2):261-71. [Medline].
- Gonzalez-Fajardo JA, Gutierrez V, San Roman JA, et al. Utility of intraoperative transesophageal echocardiography during endovascular stent-graft repair of acute thoracic aortic dissection. Ann Vasc Surg. 2002 May. 16(3):297-303. [Medline].
- Scott CH, Keane MG, Ferrari VA. Echocardiographic evaluation of the thoracic aorta. Semin Roentgenol. 2001 Oct. 36(4):325-33. [Medline].
- Von Segesser LK, Marty B, Ruchat P, et al. Routine use of intravascular ultrasound for endovascular aneurysm repair: angiography is not necessary. Eur J Vasc Endovasc Surg. 23(6):537-42. [Medline].
- Khoynezhad A, Kruse MJ, Donayre CE, White RA. Use of transcranial Doppler ultrasound in endovascular repair of a type B aortic dissection. Ann Thorac Surg. 2008 Jul. 86(1):289-91. [Medline].
- Soulen MC. Catheter angiography of thoracic aortic aneurysms. Semin Roentgenol. 2001 Oct. 36(4):334-9. [Medline].
Chest radiograph showing widening of the superior mediastinum.
Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium.
Ascending aortogram showing ascending aortic aneurysm. The patient also underwent computed tomography scanning.
Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm.
Chest radiograph in a patient with a thoracic aortic aneurysm following aneurysm surgery.
